Let’s Talk About Prolapse (Because No One Else Is)
Ever heard the term ‘prolapse’ and felt a little unsure what it meant? This article explains prolapse in simple terms, focusing on pelvic organ prolapse in women. So, let’s talk about prolapse (because no one else is).
What is Prolapse?
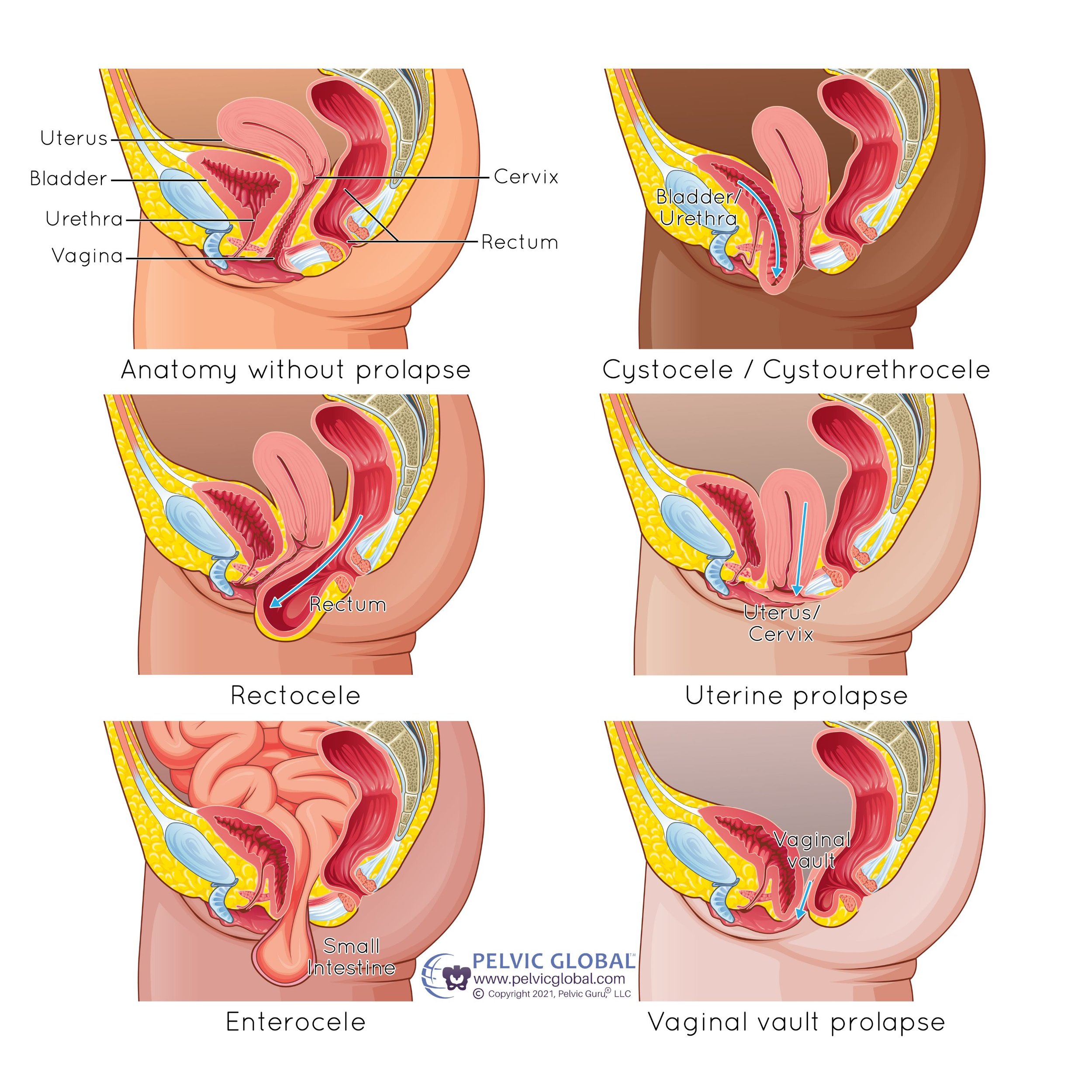
Pelvic organ prolapse is the loss of support in the pelvic floor, resulting in the downward descent of the vagina, uterus, bladder, or rectum into or through the vagina.
This loss of support can be related to an underlying dysfunction in the pelvic floor muscles, connective tissue (like ligaments), or a combination of both.
Picture a hammock that has lost some of its tension. Your pelvic floor muscles and ligaments make up the “hammock” and when pressure is applied to the top of the hammock, the hammock lowers- along with everything on top of it. In the case of the pelvic floor, the structures on top of the “hammock” include the vagina, uterus, bladder, and or rectum.
Pelvic organ prolapse is often referred to as “POP.” A prolapsed bladder (cystocele) is the most common type of pelvic organ prolapse. Men and women can experience rectocele (rectal prolapse).
What Causes Prolapse?
Pelvic organ prolapse is a common condition in women, with prevalence rates as high as 65%!
Multiple causes of prolapse have been identified. Although it is often associated with pregnancy and vaginal deliveries, prolapse also occurs in women who have never had children and those who have cesarean deliveries.
Some risk factors associated with prolapse are:
Pregnancy and childbirth
Advancing age and hormonal changes in perimenopause and menopause
Weak or overstressed pelvic floor muscles
Torn pelvic floor muscles
Chronic coughing and constipation
Heavy lifting and high-impact exercise
Connective tissue disorders and genetics
Overloading the ligaments and muscles in the pelvic floor can occur during increases in intra-abdominal pressure and high impact forces transmitted on the pelvis.
Common Symptoms of Prolapse
Many women with prolapse don’t have symptoms and are surprised to hear “you have prolapse” at a medical appointment (like I was at my recent gyn appointment!).
For those that do experience symptoms, they are most often vaginal, urinary, bowel, or sexual and can negatively impact daily activities and quality of life. These symptoms can look or feel like:
Heaviness or pressure in your pelvis
Seeing or feeling a bulge in your vagina
Feeling like something is “falling out of your vagina”
Increased frequency and urgency of urination
Leaking urine or feces, also called incontinence
Difficulty emptying your bladder or bowel
Feeling like you’re not completely emptying your bladder or bowel
Discomfort during sex
Many women notice their symptoms more towards the end of the day, when they are more fatigued, and when they have been on their feet for long periods of time.
How is Prolapse Diagnosed?
A comprehensive medical and pelvic health history along with a pelvic examination assesses prolapse, which compartments are involved, and the staging.
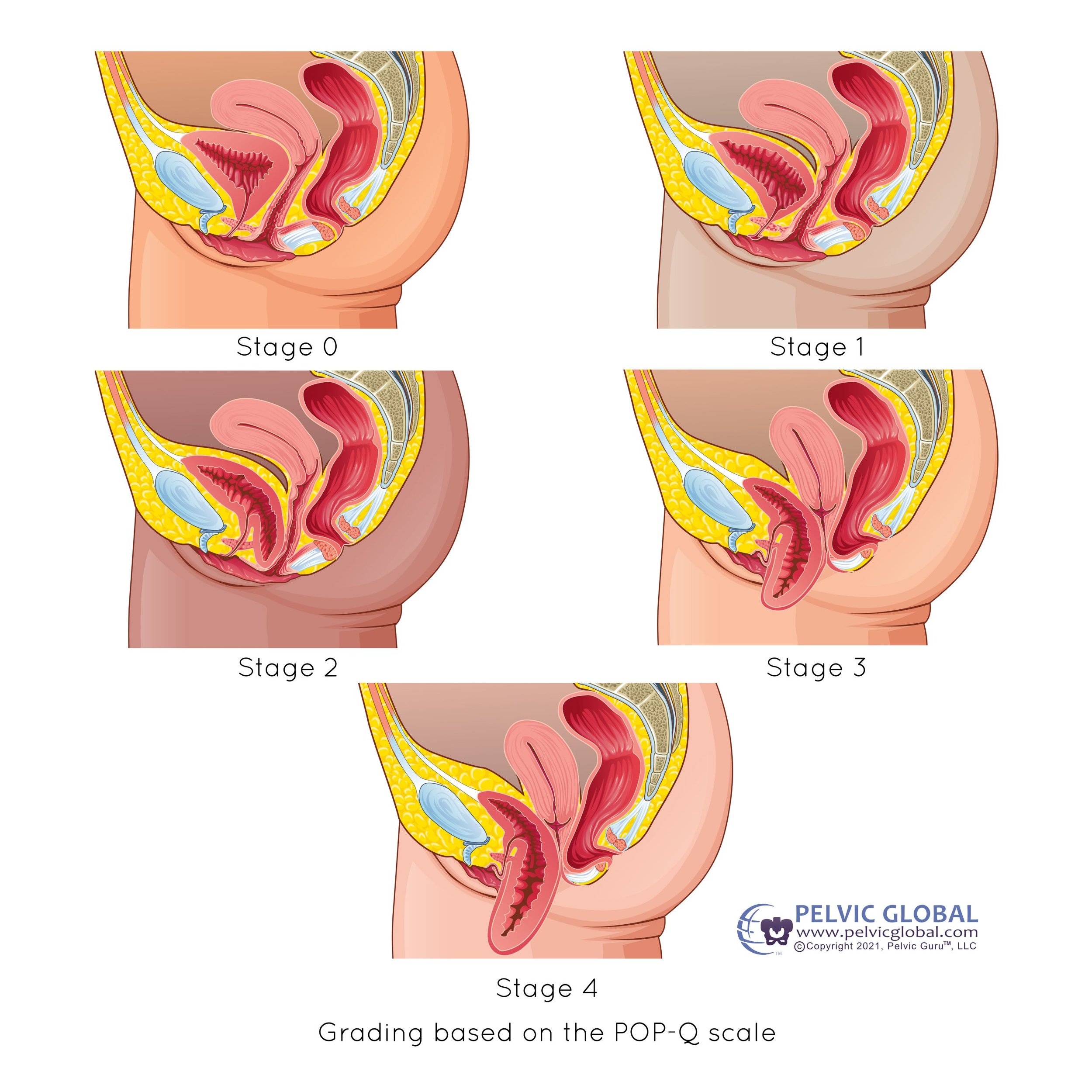
The Pelvic Organ Prolapse Quantification (POP-Q) system is often used clinically to objectively characterize prolapse and provide a “staging” or grading system in relation to the location of the hymen (thin membrane or remnant of tissue usually ~1-2 cm of the vaginal opening).
Stage 0 indicates no prolapse
Stage 1 indicates the presence of prolapse above the hymen
Stage 2 prolapse is between 1cm above and 1 cm below the hymen
Stage 3 prolapse more than 1cm below the hymen, but less than 2cm from the end of the vagina
Stage 4 is a complete eversion of the vaginal vault
In my clinic, a pelvic examination typically looks like:
A thorough discussion of your pelvic health history, symptoms, and goals
Movement, range of motion, strength, reflex, blood pressure screening
Change into gown for examination
Comprehensive external and internal examination of pelvic floor support (completed while you are laying on your back/side/stomach, and in standing, at rest when the pelvic floor structures are relaxed, and while straining)
Assessment of the strength and endurance of pelvic floor muscles
Instruction for correctly performing pelvic floor contractions
Change back into clothes you wore to the appointment
Discussion of findings, treatment options, and exercises
Bladder and bowel tracker to complete before next appointment
Schedule upcoming appointments
Treatment Options for Prolapse
Pelvic floor physical therapy and lifestyle changes are the first line treatment of prolapse!
Pelvic floor physical therapy is non-invasive, has no known serious adverse effects, and is cost effective.
Not all physical therapists are trained in the pelvic floor, so find one that is!
In my clinic, your treatment is individualized based on your goals, examination findings, and symptoms. We might learn additional information during treatment sessions to build on your examination findings! Common treatments include:
Learning how to correctly perform a pelvic floor contraction
Developing strength, endurance, and coordination of the pelvic floor muscles with
Pelvic floor dry needling to activate (or relax!) your pelvic floor muscles
Bladder training and constipation management
Fitting of a pessary, which is an intravaginal device designed to provide support to the vaginal walls (I call it a sports bra for the pelvic floor)
Lifestyle Habits That Support Pelvic Health
Drink at least 2 liters of fluids daily
Increase your dietary fiber intake to 30-40g per day
Proper toileting mechanics
Don’t strain or push down during bowel movements
Pre-contract pelvic floor muscles before sneezing, coughing, or doing high impact activities
Stay active!!!
Final Thoughts
If you have pelvic health concerns, or you’ve been told you have prolapse, you’re not alone. Prolapse is common and it’s also treatable! I understand that talking about pelvic health and seeking care can sometimes feel uncomfortable, but I assure you it’s not awkward and the empowerment from being symptom-free is worth it!
Thank you for reading Let’s Talk About Prolapse (Because No One Else Is). You can help break the stigma around prolapse and pelvic health by sharing this post.
If you are looking for pelvic and sports physical therapy services and you are located in the Colorado Springs, CO area, I’d love to help you at my clinic! Schedule an appointment and come see me in Woodland Park, where I specialize in treating pelvic floor concerns, sports injuries, and integrative dry needling.
Next on your reading list: COMING SOON!
Can I Exercise With Prolapse?
Prolapse: Exercises to Avoid
Does Running Strengthen the Pelvic Floor?
Recovery, getting back to the activities that fill your soul, and achieving peak performances ARE in your future!
References and Resources:
Bø, K., Berghmans, B., Mørkved, S., Van Kampen, M. Evidence-Based Physical Therapy For The Pelvic Floor. 3rd ed., Elsevier, 2023.
Bø, K., Anglès-Acedo, S., Batra, A. et al. Strenuous physical activity, exercise, and pelvic organ prolapse: a narrative scoping review. Int Urogynecol J 34, 1153–1164 (2023). https://doi.org/10.1007/s00192-023-05450-3
Squatty Potty for improving toileting mechanics: https://www.squattypotty.com/